Imagine this: You walk into a hospital, and the doctor pulls up your entire medical history, lab results, past treatments, imaging, and even notes from your previous specialist visits, instantly. No fumbling with CDs, no delays, no missing pieces. That’s the promise of healthcare interoperability in practice.
Yet in the many systems and institutions that make up modern medicine, data is often trapped in silos. Department by department, hospital by hospital, each piece of software speaks its own language.
How can we tear down these walls and turn fragmentation into synergy? That’s the topic here, and how your organization or clinic can use healthcare interoperability solutions to transform daily care delivery.
First of all, let’s talk about the basics. What is interoperability in the healthcare sector? In easy words, it is the capacity of various health information systems, devices, or applications to interchange data and carry out all the necessary processes such as understanding and using it in a significant way.
To put it simply, in a healthcare context, interoperability implies:
And, ideally, the whole process is secure, fast, and automated.
Thus, the data exchange in the healthcare sector is not about “sending files” merely; rather, real interoperability signifies EHR integration and the clinically meaningful data being exchanged across systems without any barriers.
Standards make this possible. Among the most important is HL7 (Health Level Seven International). HL7 defines a suite of standards, including HL7 v2, HL7 v3 / CDA, and FHIR (Fast Healthcare Interoperability Resources). FHIR is increasingly popular because it uses web-friendly formats (JSON, XML) and has modern APIs, making it a bridge between legacy systems and newer applications.
In short: healthcare interoperability is the backbone that enables all systems to “speak the same language”, unlocking the power of unified data rather than isolated silos.

If building integration sounds like a lot of work (and it is!), why do it? The benefits are compelling and when you outsource the healthcare support services, the benefits that they provide you are even better:
When the providers are able to get a patient’s complete medical history, medications, allergies, lab results, imaging, and so on, from any facility, clinical decisions are really more informed. That implies fewer mistakes, fewer tests that have been done already, and quicker interventions.
Organizations can save both time and money by eliminating duplicate tests, reducing administrative drag, and cutting data re-entry. Interoperability not only hurries up the workflows but also allows the workers to look after the patients and not to run after the documents.
Patients are often visiting various clinics, hospitals, laboratories, radiology centers, specialists, etc. When all the points in that chain are enabled to communicate and access patient data, care transitions are made less troublesome and, thus, more secure.
Data can be accessed freely, hence you can also add analytics, AI, population health tools, predictive modeling, and the like. Richer data justifies smarter insight if the systems are interoperable.
Most of the regulatory frameworks today require or at least encourage interoperability and patient data access. Furthermore, the interoperable systems give patients the power to see, share, or even contribute to their own records across different platforms.
Here’s a reality check: as of 2023, 70% of U.S. hospitals engaged in all four key domains of interoperable exchange (send, receive, find, integrate), a big increase from prior years.
And in 2021, 88% of hospitals were electronically sending or obtaining patient health information, and nearly 3/4 were integrating that data into their EHRs.
That said, adoption still isn’t universal, and many smaller or rural hospitals lag behind. The value is clear, but the path isn’t always easy.
Let’s get honest: making interoperability happen is hard. Some of the key hurdles include:
The various healthcare institutions still rely upon outdated systems or particular software that was not designed to ensure interoperability. The vendors usually rely on their own proprietary protocols thereby complicating the integration further.
Even if the systems are compliant with HL7 or FHIR, the differences in implementation, the use of optional fields, or the interpretation of the underlying meaning can bring about mismatches. The standards are really strong, but still they allow for deviating practices.
Sharing data may not be acceptable to some departments or institutions, due to privacy fears, competition for incentives, or data ownership issues.
The process of sharing health data is very demanding in terms of security, encryption, identity controls, and patient consent. Moreover, you have to ensure that you comply with the laws such as HIPAA compliance, GDPR, or local health data acts.
Building interoperable systems requires investment, not just in software, but in integration, mapping, testing, maintenance, and governance. For example, integrating a medical device to an EHR might cost thousands per unit and carry ongoing maintenance expenses.
It’s not enough to send a field called “blood pressure”; systems must agree on units, codes, and interpretation. Semantic alignment and ontology mapping are intricate tasks.
Despite the challenges, it’s precisely the organizations that take interoperability seriously and invest in robust healthcare interoperability software and solutions that will create sustained value.
What does a real-world interoperability solution look like? Below are some of the tools and approaches you can adopt (or look for in a software partner):
These act as translators, receiving HL7 v2 messages (e.g. lab results, ADT events) and routing them to appropriate systems or transforming them for compatibility.
FHIR (a standard under HL7) offers APIs for reading, writing, and querying medical data resources (Patient, Observation, Condition, etc.). Middleware platforms help unify data flows across legacy systems.
It connects different systems through adapters at one central point and also manages the data interchange in common formats.
Networks that could be either at the regional or national level and that make it possible for data to be exchanged between different organizations.
Makes sure that every patient is given a unique identifier across different systems, thus preventing the occurrence of duplicates or errors.
Convert the various coding systems used (for instance, SNOMED, LOINC, ICD) into one another so as to allow for semantic interoperability.
For governance, audit trails, encryption, and enforcing patient permissions or consent flags to minimize cybercrimes.
Once data is flowing, you can feed it into deeper layers for insights, AI, or reporting.
When your software solution combines multiple of these capabilities in a modular, secure, scalable way, with seamless EHR integration, that’s when you get real leverage. We build precisely such architectures, healthcare interoperability software that bridges gaps rather than reinforcing them.
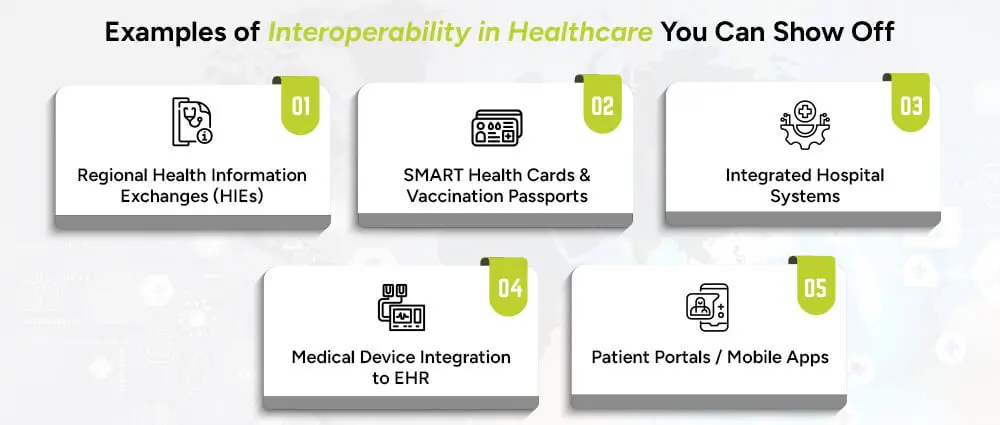
Here are a few compelling, real-world examples:
An HIE connects hospitals, labs, imaging centers, pharmacies, and clinics in many areas. In addition to that, doctors can make queries and get patient summaries from other institutions that are part of the program.
The COVID-19 pandemic brought about the need for digital vaccination records that could be verified cross-site, using HL7 FHIR and W3C frameworks, and thus the standardization of digital records was established.
A doctor’s EHR sends a patient’s laboratory orders to the laboratory’s system; results are then automatically read and added to the patient’s record without any human intervention.
The EHR receives streaming data from a ventilator, ECG machine, or infusion pump; the clinicians can monitor and notify them on one dashboard.
Patients have access to their records, lab results, or vaccination history and can even share that information with another provider, regardless of institutions and platforms.
Each of these examples is more than just cool tech, they translate isolated records into actionable care.
Here’s a suggested roadmap to make interoperability a reality (and not just a buzzword).
Map out systems, data flows, silos, standards. Use an interoperability maturity model (e.g. HIMSS) to benchmark.
What data is critical to exchange (labs, imaging, medications)? Which workflows suffer most from silos?
Align on HL7/FHIR, messaging protocols, API design, and vendor-neutral integration.
Look for modular, scalable interoperability frameworks. Look for healthcare solutions that are built this way!
Start with limited exchanges (e.g. lab to EHR), test mappings, data quality, consent flows, security controls.
Create a policy framework around data ownership, consent, versioning, and semantic semantics.
Add new systems, institutions, device integrations, and analytics layers. Monitor and refine.
If you follow this path and choose the right healthcare interoperability solutions, you’ll convert isolated silos into value-generating networks, benefiting providers, patients, and administrators
Interoperability in healthcare is not only a technical upgrade, it is a total shift towards care that is smarter, safer, and connected. The communication between hospitals, labs, and digital platforms without any effort ensures that the healthcare process is fast, reliable, and patient-centered. However, the achievement of this level of flawless connectivity requires the perfect technology partner, one who is fully aware of both the integration of EHRs and the challenges of data exchange in healthcare on a practical basis.
We at Arpatech, a company specializing in providing healthcare interoperability software, help overcome the data silos issue, support the HL7 and FHIR standards, and allow the secure and smooth flow of data across your systems. Our team is capable of providing you with the customized healthcare interoperability solutions, API development, or complete integration of your existing platforms that you need and also helping you design a scalable ecosystem that changes the way your organization delivers care.
Let’s build connected healthcare together. Get in touch with Arpatech today to discover how interoperability can unlock the full potential of your data.
Interoperability, in simple terms, aims to turn scattered data into a unified clinical story. Due to the complexities and multi-institutional nature of healthcare, it is not possible for a single system to contain everything. If interoperability is not in place:
However, if there is proper interoperability, you will have safer, faster, and smarter care.
This is a useful framework to understand how deep your connectivity is. The three main types are:
The ability of systems to pass data back and forth, wiring, protocols, message formats. For example, an HL7 v2 message moving from Lab System A to EHR B.
Ensuring that the receiving system can interpret that data in the same way the sender intended, for instance, anemia coded the same way, units matched, terminology aligned. It’s about shared meaning, e.g. SNOMED, LOINC, standard terminologies.
Aligning workflows, policies, consent, permissions, responsibilities across institutions. It involves governance, data ownership, authentication, business rules. Even if two systems speak the same language, they need agreements about who’s allowed to fetch what, when, and how.
When all three are working, you have truly interoperable healthcare, not just data passing, but data that leads to action.