Remote patient monitoring software is becoming a strategic imperative in the healthcare industry. Health systems, clinics, telehealth companies and startups alike are asking how to develop a remote patient monitoring software that scales, that stays secure, that meets both providers and patients where they are.
Let’s dive into how you can build a remote patient monitoring software system that’s future-ready, metrics-driven and designed for scale.
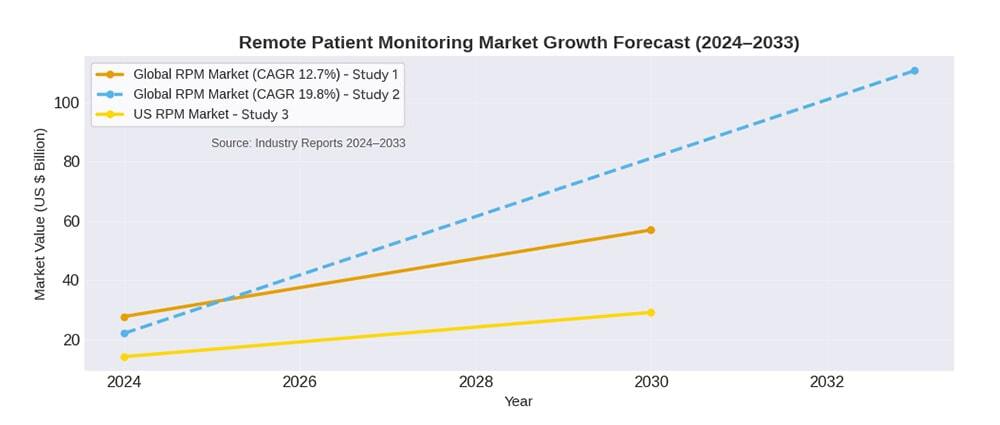
First: let’s look at the numbers. The global market for remote patient monitoring is growing at a fierce pace. According to one report, the global RPM market stood at US $27.72 billion in 2024 and is projected to reach US $56.94 billion by 2030, representing a CAGR of around 12.7%.
Another puts the market at about US $22.03 billion in 2024, with expectations to reach over US $110.71 billion by 2033, or a CAGR near 19.8%. In the U.S. alone, the value of the remote patient monitoring market is forecasted to jump from about US $14.15 billion in 2024 to US $29.13 billion by 2030.
So, if your organization (or your clients) is asking: “How do we pick the best remote patient monitoring software, or become one of the remote patient monitoring software providers ourselves?”, you’re in the right place. Let’s break it down.
Before diving into architecture, you must answer some key questions:
What do we mean by “What is Remote Patient Monitoring”?
Put simply, RPM refers to technology-enabled care that collects patient data outside of traditional clinical settings (for example, in the home), transmits that data to healthcare providers, and allows interventions based on that data.
So, here are the questions you need to ask yourself before starting:
Writing this down early ensures that when developers ask “What features? What integrations? What scale?” you have metrics and business justifications.
When you ask: How to build a remote patient monitoring software, scale becomes a core consideration. Here’s what you’ll want to include:
You’ll want to connect to multiple devices (wearables, vital-sign monitors, implantables, home-health sensors). The more device types you support, the broader your market.
Support streaming, batch uploads, and offline data sync.
Ensure interoperability standards, HL7 FHIR, Bluetooth LE, WiFi, cellular, are addressed.
Use a cloud-based remote patient monitoring software architecture: it gives you automatic scale, geographic redundancy, and pay-as-you-go infrastructure.
Segment your services: device ingestion, data storage, analytics/AI, notification engine, user access (clinician and patient).
Apply multi-tenant design if you expect multiple clients or organisations, or enable healthcare cloud migration.
The volume of data is high. You’ll need logic that turns raw vital-sign data or symptom data into meaningful alerts, trends, risk scores.
AI/ML modules for predictive monitoring (for example, escalating risk of readmission) are becoming a differentiator in the market.
Medical data is sensitive. Compliance with HIPAA (USA), GDPR (EU), local health-privacy laws is mandatory. Use encrypted data-in-transit and at rest, secure device onboarding, role-based access control.
Audit logs, identity management, strong authentication.
EHR/EMR integration, telehealth platform connection (which brings us to telehealth vs RPM), billing/revenue cycle systems for remote care reimbursement.
If you’re evaluating existing options or looking to outsource a healthcare remote patient monitoring software developer, focus on these differentiators:
Can the system be customized for different care-pathways? If you need to develop a remote patient monitoring software for a niche (say renal care, post-surgery, chronic heart failure), flexibility is key.
Understand the remote patient monitoring software pricing: SaaS vs perpetual license, per-device/per-user, tiered usage.
Can the system handle thousands or millions of patients/devices?
Many clients prefer cloud-based remote patient monitoring software for ease of updates and remote management.
Providers increasingly want data on outcomes (reduced readmissions, improved adherence) to justify ROI.
The best remote patient monitoring software plays well with other systems meaning the healthcare interoperability between systems like EHRs, telehealth, and mobile apps.
Partnerships with device vendors, analytics companies, telehealth platforms strengthen your value proposition.
One common question: “What is the cost of remote patient monitoring software?” Cost is multi-factorial: number of patients/devices, complexity of workflows, integrations, regulatory compliance, customizations, hosting model, IT support, maintenance.
According to our expert opiion:
There’s no one-size-fits-all “price list” for “software for remote patient monitoring” or “remote patient monitoring software system” given the variations. That’s why building modular and scalable is key, it allows costs to scale more predictably.
Because, let’s be honest: technology is useful, but adoption is critical. A high-performing system means nothing if clinicians and patients don’t use it. Some tactics:
When you think of building a scalable RPM system, you’ll frequently hear the term “telehealth platforms” alongside it. While closely connected, they serve different roles. We’ll look at the difference below, but for now understand: a robust remote patient monitoring software development project will integrate seamlessly with telehealth to provide a full-care experience: data collection + virtual consultation + intervention.
Since you’re building something scalable and transactional, you’ll want to monitor these KPIs:
When you’re discussing a project or prospect for best remote patient monitoring software, these metrics help demonstrate ROI and scalability.
If you are contemplating to become a provider or choosing one that offers remote patient monitoring software, the first thing to consider is: the market is full of sellers, so it is vital to differentiate yourself:
When you mention “remote patient monitoring software providers,” these are the features that make you different from the rest.
Here are some practical tips gleaned from real-world cases:
Select a small cohort of patients, monitor data flows, clinician engagement, patient behaviour.
Patients hate complicated device set-ups. Use plug-and-play as much as possible.
New dashboards can disrupt workflows; invest in change management.
Build your compliance, privacy, consent systems from day one. Retrofitting is expensive.
Auto scaling, auto updates, logging/monitoring.
Show them trends and outcomes (not just raw device data) and build for localization and different regulatory regimes if you will scale globally.
Remote monitoring and telehealth technologies evolve fast; you want a modular code base.
Without sufficient patient engagement, your system won’t deliver value.
Device vendors, telehealth vendors, and analytics vendors often form ecosystems; join them rather than reinvent everything.
If your organization is ready to step into this space, to build a remote patient monitoring software or upgrade an existing platform, now is an excellent time. With a growing global market, increasing demand from chronic-disease care and home-care models, and telehealth becoming mainstream, your opportunity is large.
At Arpatech, we specialise in remote patient monitoring software development and can help you every step of the way: from concept and architecture to deployment and scaling. Whether you’re looking to develop a remote patient monitoring software from scratch or integrate enhanced features into an existing system, we can guide you through technology choices, cloud-based deployment, regulatory compliance, and user adoption.
Let’s build your next-generation remote patient monitoring platform together, one that delivers outcomes, scales effortlessly, and positions you as a leader among remote patient monitoring software providers.
There is no single answer, because cost depends on number of patients/devices, feature scope, integrations, regulatory complexity, deployment model (cloud vs on-premises). As noted above, for a full custom build, you might expect budgets to be on a little higher side.
On a per-patient SaaS basis, some packaged solutions may charge hundreds of dollars per patient per year. The key is to define the scope clearly and build modularly so you can add features as you scale.
Yes, from both a care-delivery and business perspective. The data shows strong growth in uptake and market size, and the ability to monitor patients outside the hospital enables lower costs, better outcomes (reduced readmissions, earlier interventions), greater patient reach.
If implemented well (with good UX, clinician buy-in, patient adherence), remote patient monitoring can provide a real competitive advantage and cost savings.
In short: telehealth is a broader umbrella term covering virtual visits, tele-consultations, remote delivery of healthcare services via audio/video. Remote patient monitoring is a subset focused on monitoring patient health data remotely (such as vital signs, device data, symptoms) outside a traditional clinical setting, and acting on insights from that data.
They work together: RPM collects the data, telehealth enables the intervention. But they are distinct in terms of workflow, requirements and technology.